ABPM is a non-invasive method of obtaining blood pressure readings over a 24-hour period, whilst the patient is in their own environment (home and/or work), representing a true reflecton of their blood pressure.
The ABPM can be programmed to automatically measure the blood every 15 minutes, 30 minutes, 60 minutes, or more, based on the doctors discretion; one hour measurements are most commonly used.
ABPM is considered more accurate and reliable for determining who has hypertension (high blood) than the readings taken by the nurse or doctor in the clinic setting.

A holter monitor is a battery-operated portable device that measures and records your heart’s activity (ECG) continuously for 24 to 48 hours or longer depending on the type of monitoring used. The device is the size of a small camera. It has wires and small electrodes that attach to your skin. The holter monitor records your ECG as you go about your daily activities.
There are no risks to wearing one and it causes no pain or discomfort. Removing of electrodes after monitoring can cause some mild skin irritation.

Spirometry is a common office test used to assess how well your lungs work by measuring how much air you inhale, how much you exhale and how quickly you exhale.
It may also be used to periodically to check whether a treatment for a chronic lung condition is helping you breathe better.
Your doctor may suggest a spirometry test if he or she suspects your signs or symptoms (acute or chronic cough; difficulty breathing; shortness of breath) may be caused by a chronic lunch condition such as:
Accurate and objective Peripheral Arterial Disease diagnosis

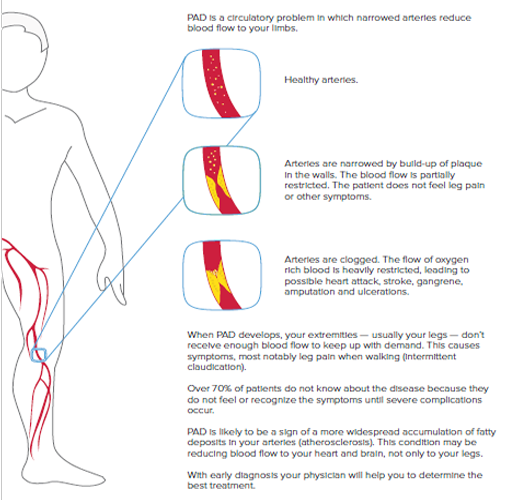
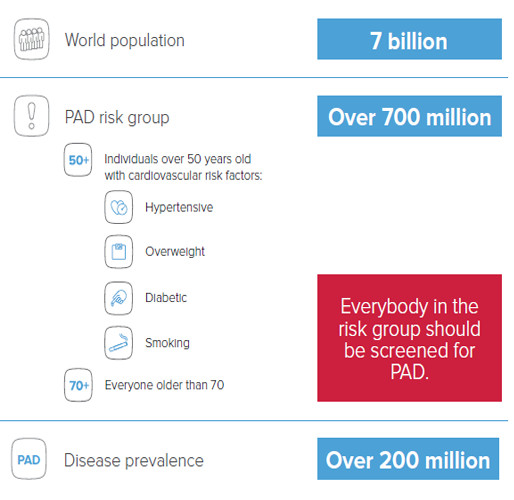
Ankle-Brachial Index (ABI) is a very simple comparison of blood pressures in legs and arms. It is non-invasive and painless. With MESI ABPI MD the procedure becomes reliable, objective and even possible to be performed as screening in first-contact healthcare. ABI screening is incredibly important for at least two reasons:
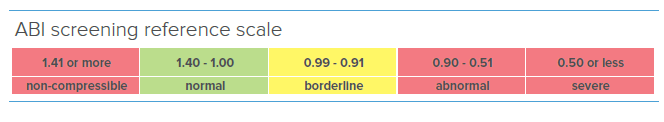
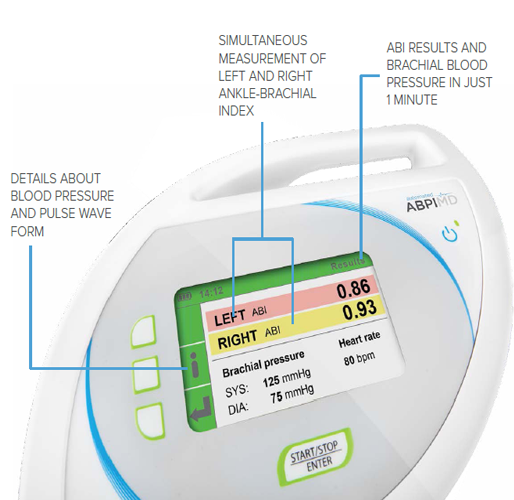
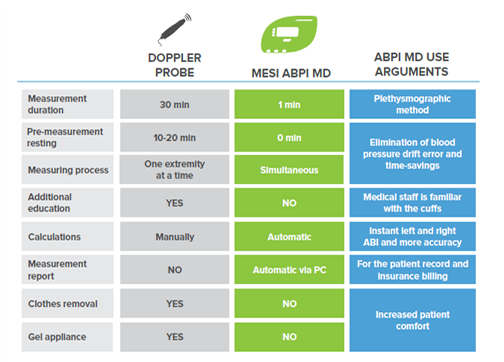
Compared to the handheld Doppler probe, MESI ABPI MD performs an automated ABI measurement. Innovative technology enables the device to provide accurate and objective results, based on which the physicians can diagnose Peripheral Arterial Disease with great confidence.
Smart software prevents false results even in the case of critical ischemia or medial calcinosis, and gives physicians all the confidence they need.
It is not possible to measure blood pressure in ankles with a brachial blood pressure device. Therefore our algorithm is different, developed with human ankle anatomy in mind.
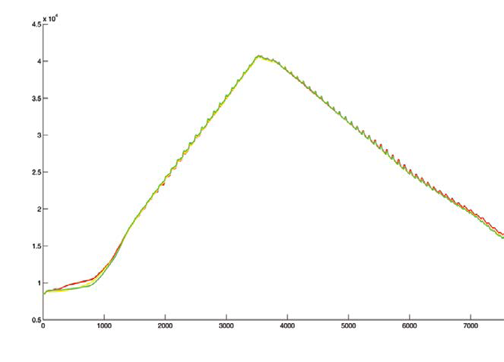
Plethismograpy sensors detect the smallest changes in volume. Ease-of-use excludes the possibility of human error as well as there is no need for additional training
Because blood pressure is constantly changing, simultaneous measurement is crucial to avoid error from blood pressure drift.
Unique error detection without false results
Thanks to a unique error detection system, MESI ABPI MD will alert the operator of any irregularities, which have occurred during the measurement process.
If the cuffs have been poorly placed or if the patient has been moving during the measurement, the error message will be displayed on the screen.
It is crucial to provide a reliable measurement also when examining a patient with severe PAD. Our improved plethysmographic sensors detect critical ischemia and medial calcinosis even when pressure oscillations are not available due to heavy occlusion. Every measurement with MESI ABPI MD provides sufficient information for further actions.
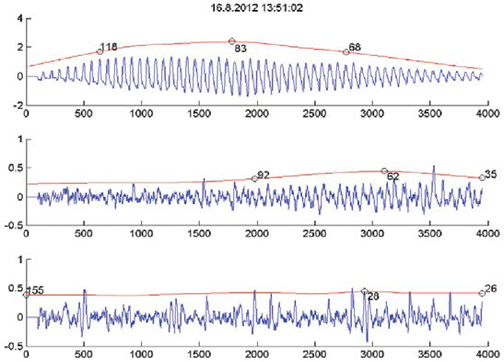
While performing the measurement on a patient with severe PAD, it is possible that no pulse is detected. The obstruction of the artery is heavy, resulting in weak blood flow after the obstruction. The pressure is supressed and the difference between systolic and diastolic pressure vanishes.
Elimination of blood pressure drift error
It is crucial to eliminate the delay between separate measurements on each extremity to achive maximum ABI accuracy.
MESI ABPI MD conducts simultaneous blood pressure measurements on all extremities.

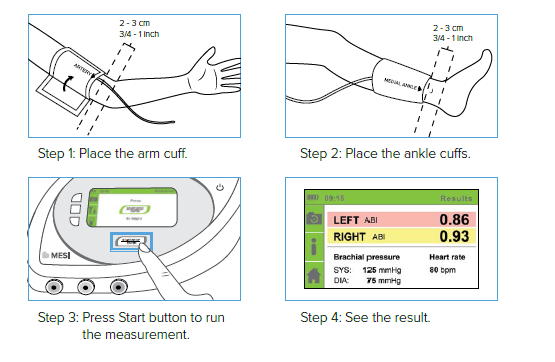
Cuffs are essential for the ABI measurement
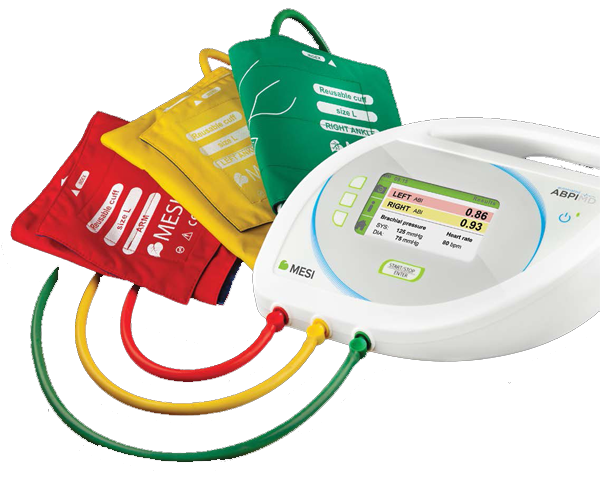
Conical shape of the cuffs provides perfect fitting to patient’s extremities, providing the best accuracy.
Different colours indicate where to place each cuff.
The red cuff should be positioned on the upper arm, green on the right and yellow on the left ankle.
Each cuff is clearly labelled and includes a diagram to ensure correct placement. No training is needed as comprehensive guidelines are provided.
Cuffs are available in medium and large sizes.
2 in 1 : ABI and BP measurements
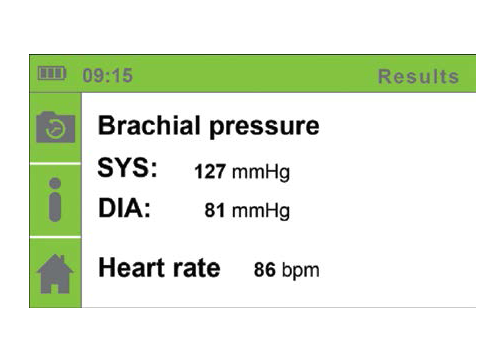
Expertly developed MESI ABPI MD enables two measurement modes:

Stand supplements MESI ABPI MD
The place for MESI ABPI MD is next to the examination bed. A stand with magnetic base has been designed to hold both – the device and the cuffs.
The stand enables the device to be easily portable and significantly helps with the durability of the device and the cuffs respectively.

Long lasting battery for maximum portability During the measurement, patient needs to be lying down. Examination beds are not always next to the electrical sockets, which is why MESI ABPI MD is equipped with a long lasting rechargeable battery.

MESIresults application comes free with the device. MESI ABPI MD can be connected to a computer to provide an electronic copy or a printout of the ABI result. MESIresults also enables information such as name, address and logo of the healthcare institution to be imported into every measurement report.